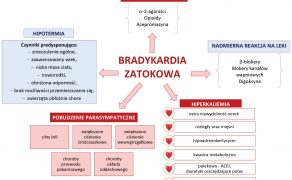
Bradykardia zatokowa u psów
Piśmiennictwo
- Amon T., Kästner S.B.R., Kietzmann M., Tünsmeyer J.: Plasma levels of a methadone constant rate infusion and their corresponding effects on thermal and mechanical nociceptive thresholds in dogs. „BMC Vet Res”, 2021, 17, 35.
- Bainbridge F.A.: The influence of venous filling upon the rate of the heart. „J Physiol”, 1915, 50, 65-84.
- Bellini L., Perazzi A., Carobbi B., Iacopetti I.: Maxillomandibulocardiac reflex in a dog. „Acta Vet Scand”, 2018, 60, 64.
- Benchekroun G. et al.: Dogs with macroadenomas have lower body temperature and heart rate than dogs with microadenomas. „Vet J Lond Engl”, 2017, 227, 42-45.
- Boettcher D.H., Zimpfer M., Vatner S.F.: Phylogenesis of the Bainbridge reflex. „Am J Physiol”, 1982, 242, R244-246.
- Bomassi E. et al.: Atrial cardiomyopathy in an adult Labrador retriever dog. „Schweiz Arch Tierheilkd”, 2017, 159, 594-599.
- Caliskan K., Balk A.H.M.M., Jordaens L., Szili-Torok T.: Bradycardiomyopathy: the case for a causative relationship between severe sinus bradycardia and heart failure. „J Cardiovasc Electrophysiol”, 2010, 21, 822-824.
- Chanan-Khan A. et al.: Complement activation following first exposure to pegylated liposomal doxorubicin (Doxil): possible role in hypersensitivity reactions. „Ann Oncol Off J Eur Soc Med Oncol”, 2003, 14, 1430-1437.
- Crystal G.J., Salem M.R.: The Bainbridge and the ‘reverse’ Bainbridge reflexes: history, physiology, and clinical relevance. „Anesth Analg”, 2012, 114, 520-532.
- Davis J., Raisis A.L., Haitjema H., Drynan E.A., Hosgood, G.L.: Paradoxical bradycardia during surgical caudal vena cava occlusion in an anesthetized dog. „J Vet Emerg Crit Care San Antonio Tex”, 2017, 27, 243-249.
- Fabritz L. et al.: Gene dose-dependent atrial arrhythmias, heart block, and brady-cardiomyopathy in mice overexpressing A(3) adenosine receptors. „Cardiovasc Res”, 2004, 62, 500-508.
- Fisher E.W.: Fainting in Boxers – the possibility of vaso-vagal syncope (Adams-Stokes attacks). „J Small Anim Pract”, 1971, 12, 347-349.
- Flood J.A., Hoover J.P.: Improvement in myocardial dysfunction in a hypothyroid dog. „Can Vet J”, 2009, 50, 828-834.
- Gallay J. et al.: Cardiac leiomyoma associated with advanced atrioventricular block in a young dog. „J Vet Cardiol Off J Eur Soc Vet Cardiol”, 2011, 13, 71-77.
- Goette A. et al.: EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. „Eur Eur Pacing Arrhythm Card Electrophysiol J Work Groups Card Pacing Arrhythm Card Cell Electrophysiol Eur Soc Cardiol”, 2016, 18, 1455-1490.
- Goodman I. H.: Survival of a dog with accidental colchicine overdose. „J Vet Emerg Crit Care San Antonio Tex”, 2020, 30, 74-80.
- Gunasekaran T., Olivier N.B., Smedley R.C., Sanders R.A.: Pericardial Effusion in a Dog with Pericardial Hemangiosarcoma. „J Vet Cardiol Off J Eur Soc Vet Cardiol”, 2019, 23, 81-87.
- He W. et al.: Sympathetic mechanisms in an animal model of vasovagal syncope. „Clin Auton Res Off J Clin Auton Res Soc”, 2018, 28, 333-340.
- Jarisch A., Richter H.: Die afferenten bahnen des veratrine effektes in den herznerven. „Arch Exp Pathol Pharmacol”, 1939, 193, 355-371.
- Johnson M.S., Martin M.W. S., Henley W.: Results of pacemaker implantation in 104 dogs. „J Small Anim Pract”, 2007, 48, 4-11.
- Kogika M.M., de Morais H.A.: A Quick Reference on Hyperkalemia. „Vet Clin North Am Small Anim Pract”, 2017, 47, 223-228.
- Li G.B., Lu G.X.: Gene Delivery Efficiency in Bone Marrow-derived Dendritic Cells: Comparison of Four Methods and Optimization for Lentivirus Transduction. „Mol Biotechnol”, 2009, 43, 250-256.
- Lu W. et al.: mHCN4 genetically modified canine mesenchymal stem cells provide biological pacemaking function in complete dogs with atrioventricular block. „Pacing Clin Electrophysiol”, 2013, 36, 1138-1149.
- Mari L., Shea A.: Symptomatic Narcolepsy/Cataplexy in a Dog with Brainstem Meningoencephalitis of Unknown Origin. „J Am Anim Hosp Assoc”, 2020, 56, e56201.
- McGrath C.A., Borgeat K., Wilson H.E.: Third-degree atrioventricular block with narrow QRS complexes in a case of hypoadrenocorticism in a dog. „J Small Anim Pract”, 2021. DOI: 10.1111/jsap.13464.
- McMillan M.W., Aprea, F., Leece E.A.: Potential Bezold-Jarisch reflex secondary to a 180° postural change in an anaesthetized dog. „Vet Anaesth Analg”, 2012, 39, 561-562.
- Nobre Pacifico Pereira K.H. et al.: Neonatal sepsis in dogs: Incidence, clinical aspects and mortality. „Theriogenology”, 2022, 177, 103-115.
- Oberg B., Thorén P.: Increased activity in left ventricular receptors during hemorrhage or occlusion of caval veins in the cat. A possible cause of the vaso-vagal reaction. „Acta Physiol Scand”, 1972, 85, 164-173.
- Oberg B., White S.: The role of vagal cardiac nerves and arterial baroreceptors in the circulatory adjustments to hemorrhage in the cat. „Acta Physiol Scand”, 1970, 80, 395-403.
- Parisi C., Phillips V., Ferreira J., Linney C., Mair A.: Anaesthetic management and complications of transvascular patent ductus arteriosus occlusion in dogs. „Vet Anaesth Analg”, 2020, 47, 581-587.
- Perego M. et al.: Heart rhythm characterisation during unexplained transient loss of consciousness in dogs. „Vet J Lond Engl”, 2020, 263, 105523.
- Pöntinen P.J.: The importance of the oculocardiac reflex during ocular surgery. „Acta Ophthalmol (Copenh)”, 1966, 86, 1-66.
- Pugliese M. et al.: Electrocardiographic Findings in Bitches Affected by Closed Cervix Pyometra. „Vet. Sci.”, 2020, 7, E183.
- Robinson K. et al.: A Pilot Study on the Safety of a Novel Antioxidant Nanoparticle Delivery System and Its Indirect Effects on Cytokine Levels in Four Dogs. „Front Vet Sci”, 2020, 7, 447.
- Ryane E.: Englar. Common Clinical Presentations in Dogs and Cats. Wiley-Blackwell, 2019.
- Sanders P., Kistler P.M., Morton J.B., Spence S.J., Kalman J.M.: Remodeling of sinus node function in patients with congestive heart failure: reduction in sinus node reserve. „Circulation”, 2004, 110, 897-903.
- Santilli R.N. Moise S., Pariaut R., Perego M.: Electrocardiography of the dog and cat. Diagnosis of arrhythmias. EDRA S.p. A., 2018.
- Santilli R.A., Giacomazzi F., Porteiro Vázquez D.M., Perego M.: Indications for permanent pacing in dogs and cats. „J Vet Cardiol Off J Eur Soc Vet Cardiol”, 2019, 22, 20-39.
- Schaller B., Probst R., Strebel S., Gratzl O.: Trigeminocardiac reflex during surgery in the cerebellopontine angle. „J Neurosurg”, 1999, 90, 215-220.
- Swanson L.E., Huibregtse B.A., Scansen B.A.: A retrospective review of 146 active and passive fixation bradycardia lead implantations in 74 dogs undergoing pacemaker implantation in a research setting of short term duration. „BMC Vet Res”, 2018, 14, 112.
- Szebeni J.: Complement activation-related pseudoallergy: a new class of drug-induced acute immune toxicity. „Toxicology”, 2005, 216, 106-121.
- Szebeni J.: Complement activation-related pseudoallergy: a stress reaction in blood triggered by nanomedicines and biologicals. „Mol Immunol”, 2014, 61, 163-173.
- Świątnicki W., Wolski C., Woźniakowski B., Rotkiewicz A., Zawirski M., Tybor K.: Anatomiczne podstawy i kliniczne następstwa odruchu trójdzielno-sercowego. „Postępy Psychiatrii i Neurologii”, 2009, 18 (2), 195-199.
- Teske E., Rutteman G.R., Kirpenstein J., Hirschberger J.: A randomized controlled study into the efficacy and toxicity of pegylated liposome encapsulated doxorubicin as an adjuvant therapy in dogs with splenic haemangiosarcoma. „Vet Comp Oncol”, 2011, 9, 283-289.
- Tsompanidou P.P., Kazakos G.M., Anagnostou T.L.: Dopamine-induced bradycardia in two dogs under isoflurane anaesthesia. „J Small Anim Pract”, 2013, 54, 672-674.
- Une Y., Furusawa N., Shirota K., Nomura Y.: Atrial adipofibrosis in a dog. „J Vet Diagn Investig Off Publ Am Assoc Vet Lab Diagn Inc”, 1998, 10, 192-194.
- Végh A.M.D. et al.: Cardiomyocyte Progenitor Cells as a Functional Gene Delivery Vehicle for Long-Term Biological Pacing. „Mol Basel Switz”, 2019, 24, E181.
- Végh A.M.D. et al.: Toward Biological Pacing by Cellular Delivery of Hcn2/SkM1. „Front Physiol”, 2020, 11, 588679.
- von Bezold A.V., Hirt L.: Uber die physiologischen wirkungen des essigsauren veratrins. „Untersuchungen aus dem Physiologischen Laboratorium Wurzburg”, 18671, 75-156.
- Ward J., McLaughlin A., Burzette R., Keene B.: The effect of a surgical safety checklist on complication rates associated with permanent transvenous pacemaker implantation in dogs. „J Vet Cardiol Off J Eur Soc Vet Cardiol”, 2019, 22, 72-83.
- Wesselowski S., Cusack K., Gordon S.G., Jeffery N., Saunders A.B.: Artificial cardiac pacemaker placement in dogs with a cohort of myocarditis suspects and association of ultrasensitive cardiac troponin I with survival. „J Vet Cardiol Off J Eur Soc Vet Cardiol”, 2019, 22, 84-95.
- Zhou X., Hohman A., Hsu W.H.: Review of extralabel use of isoxazolines for treatment of demodicosis in dogs and cats. „J Am Vet Med Assoc”, 2020, 256, 1342-1346.
- Zucker I.H., Cornish K.G.: The Bezold-Jarisch in the conscious dog. „Circ Res”, 1981, 49, 940-948.
lek. wet. Karolina Kapturska
II rok Szkoły Doktorskiej
Katedra Farmakologii i Toksykologii
Wydział Medycyny Weterynaryjnej
Uniwersytet Przyrodniczy we Wrocławiu
karolina.kapturska@upwr.edu.pl
Galeria
120
ALGORYTMY
POSTĘPOWANIA
w weterynarii
POSTĘPOWANIA
w weterynarii